Placenta | Vasa Previa
Vasa previa is a condition which arises when fetal blood vessels implant into the placenta in a way that covers the internal os of the uterus. This section outlines possible pregnancy complications associated with this condition.
Overview
In a normal pregnancy, the placenta implants at the top of the womb (uterus) in the region described as the “fundus” of the uterus. As shown in the diagram of a normal pregnancy, this allows the placenta to be out of the way to allow the developing baby to be “head-first” and therefore ready for normal birth at 9 months. Importantly, for proper placental development and a successful pregnancy, the umbilical cord needs to insert into the central part of the placental disc. Additionally, when examining the angiogram of a surface of a placenta in a healthy pregnancy (shown below), the umbilical vessels spread out evenly all over the disc, without wandering beyond the disc into the membranes. These vessels are in pairs (arteries with veins) and, as is described in Placenta 101[k1] section, they form circuits that send blood inside the placental tissue (called villi) to extract nutrients and oxygen from the mother’s blood.
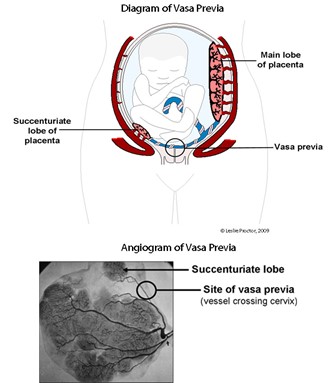
On the contrary, a placenta with the vasa previa does not exhibit the same features. As the diagram below shows, vasa previa results into the following complications:
- The umbilical cord of the developing baby does not insert into the placenta; rather, it is inserts into the membranes (known as a velamentous cord insertion);
- The main portion of the placenta is low-lying (minor placenta previa)[k1] ;
- Fetal vessels run from the velamentous cord insertion to the placenta, but to do so they have to cross the opening where the developing baby is destined to deliver (the internal os of the cervix);
- A smaller separate lobe (known as a succenturiate lobe) is seen in the lower segment; since fetal vessels also need to supply this lobe, the presence of a succenturiate lobe poses a risk for the development of vasa previa.
Causes
Vasa Previa is a disorder that is established in early pregnancy during placental formation and development.
Risk Factors
There is no risk to the developing fetus until the time of delivery. At that time, as the cervix shortens and opens in normal labour, the exposed membranes will eventually burst to release amniotic fluid – often described as “my waters have broken”. At this point, the fetal vessels may rupture. The blood lost vaginally belongs to the baby – since it has very little blood compared to the mother, it will likely either die, or survive with brain and/or kidney injury, unless an immediate Caesarean Section is done under a general anaesthetic. The same scenario can be caused by artificial rupture of the membranes by the nurse, doctor, or midwife, in early labour. The image below illustrates a placenta with vasa previa. The asterix indicates the site of rupture of the fetal vessels (image courtesy of Dr. Sarah Keating[l1] , Mount Sinai Hospital).

Generally, vasa previa is not dangerous to the mother; however, the woman must undergo a Caesarean section so that her infant is born in a healthy condition.
There are several risk factors associated with vasa previa. These include:
- IVF pregnancy
- Low lying placenta in the second trimester
- Velamentous insertion
- Bi-lobed or succenturiate-lobed placenta
- Single umbilical artery
- Multiple pregnancy (especially mono-chorionic)
Diagnosis
Ultrasound can be used to exclude or diagnose vasa previa. The optimal time is at the time of the routine fetal anatomy ultrasound examination at 18-20 weeks. This examination is done using an ultrasound probe on the pregnant belly (trans-abdominal ultrasound) though a separate internal (trans-vaginal ultrasound) examination at the same visit is normally required in order to establish the diagnosis.
Can Vasa Previa be diagnosed in labour before it’s too late to save the baby?
Yes. In normal labour, or even induction of labour, the cervix will open at least 3-4 centimeters before the membranes rupture themselves, or are ruptured by your nurse, doctor or midwife. All have been trained to be alert to recognising the rare possibility of vasa previa as pulsating vessels running across the bulging membranes. Should vasa previa be suspected this way, the woman will be transferred to the operating room for a careful clinical assessment by a senior doctor. Should vasa previa be diagnosed in this setting, an immediate Caesarean section will result in a healthy baby. Normally there is enough time to have a spinal anaesthetic for this operation.
Are pregnancies routinely screened for Vasa Previa today?
Generally no, because professional bodies guiding standards of ultrasound in pregnancy do not explicitly require that this condition be searched for. Some progress has recently been made towards the goal of universal screening for vasa previa. You may wish to ask the technologist performing your 18-20 week fetal anatomy ultrasound to take a few moments to document the placental cord root and ensure that you do not have a succenturiate lobe.
How Common is Vasa Previa?
Fortunately vasa previa is a rare condition, affecting around 1/2000 deliveries. If the condition is not suspected or diagnosed before labour and delivery, just under half will survive, whereas if the diagnosis is made, almost all (97%) will survive as they are born by planned Caesarean section (normally at 36-37 weeks) so as to avoid any risk of early labour that could rupture the vasa previa vessels. For a detailed review of vasa previa, please click here.
Management
Several management strategies have been developed over the years to ensure a safe and timely delivery of the baby, to minimize the damage which may be caused by ruptured blood vessels:
- Caesarean section: The most important step is to schedule a Caesarean section before the onset of labour. So long as the cervix is long and closed with ultrasound monitoring, we do not advocate either hospital admission or delivery prior to 35 weeks;
- Ultrasound assessment: Vasa previa does not develop into placental insufficiency[k1] , therefore, the developing baby will grow normally. Intensive ultrasound surveillance is not required; rather, the cervix should be assessed intermittently by trans-vaginal ultrasound. Under normal circumstances, this is done every 2 weeks from 24 weeks, and weekly from 32 weeks of gestation;
- Admission: We reserve antenatal admission for the following circumstances: a history of preterm delivery; risk factors for preterm delivery, including a short (<2cm) cervix, maternal anxiety not adequately managed with supportive psychotherapy, relevant maternal co-morbidities; or remote home location;
- Steroids for fetal lung maturation: We discuss and provide a standard course of maternal intra-muscular (into the buttock) steroid injections to promote fetal lung maturation, in circumstances where we believe that antenatal admission is warranted, leading to pre-term delivery (prior to 34 weeks).
Are special precautions needed at Caesarean section for vasa previa?
No, though delayed cord clamping is not possible. In the vasa previa condition, the cord is clamped immediately to secure the infant’s circulation. The omission of delayed cord clamping is not critical for term infants. Cord blood collection for stem cells is generally possible, if desired.
Do women with vasa previa need to be transferred to a high-risk pregnancy specialist?
No. The diagnosis is established by a specialist in ultrasound (radiologist and technician, or maternal-fetal medicine specialist). Thereafter, the care, including planned Caesarean section, is a standard procedure provided by trained obstetricians.
Role of placental function testing
The early detection of vasa previa is essential to guide physicians and patients to prepare for the birth of the child by planned Caesarean section. Placental ultrasound including colour Doppler [l1] assessment of the cord insertion is an effective second trimester screening method to identify placentas with velamentous insertions, or with multiple lobes that are at risk of vasa previa. Trans-vaginal ultrasound, in both real-time and colour Doppler, is used to establish or refute the diagnosis of vasa previa.
Prognosis
Vasa Previa is not a genetic condition – so it has a random recurrence risk, approximately 1/2000. Women with a previously-affected pregnancy should seek reassurance of normal placental anatomy by ultrasound in a future pregnancy.
External Links
The following links may be useful if you would like to find out more about vasa previa:
- Current guidelines on obstetric ultrasound examinations
- Royal College Obstetricians and Gynaecologist Guidelines for diagnosis and management of vasa previa
- The Vasa Previa Foundation
