Placenta | Placenta praevia
In placenta praevia, the placenta implants on the lower instead of the upper segment of the uterus, partially or completely covering the cervix. If the placenta only partially covers the cervix in mid pregnancy, it may resolve on its own by term, allowing vaginal birth. If it covers the cervix completely, birth must be by Caesarean section.
Essential Information
- Accurate diagnosis and appropriate management of placenta praevia results in a favourable outcome for the vast majority of women with this condition.
- In most cases, placenta praevia is found at the time of the routine abdominal ultrasound exam at 18-20 weeks. A transvaginal ultrasound may be required to confirm the diagnosis.
- Placenta praevia can cause bright red vaginal bleeding in the second half of pregnancy. The bleeding may range from light to heavy, and may be accompanied by uterine cramping, but is typically not associated with abdominal pain.
- In complete placenta praevia, birth must be by Caesarean section.
Overview
There are 4 types of placenta praevia as follows: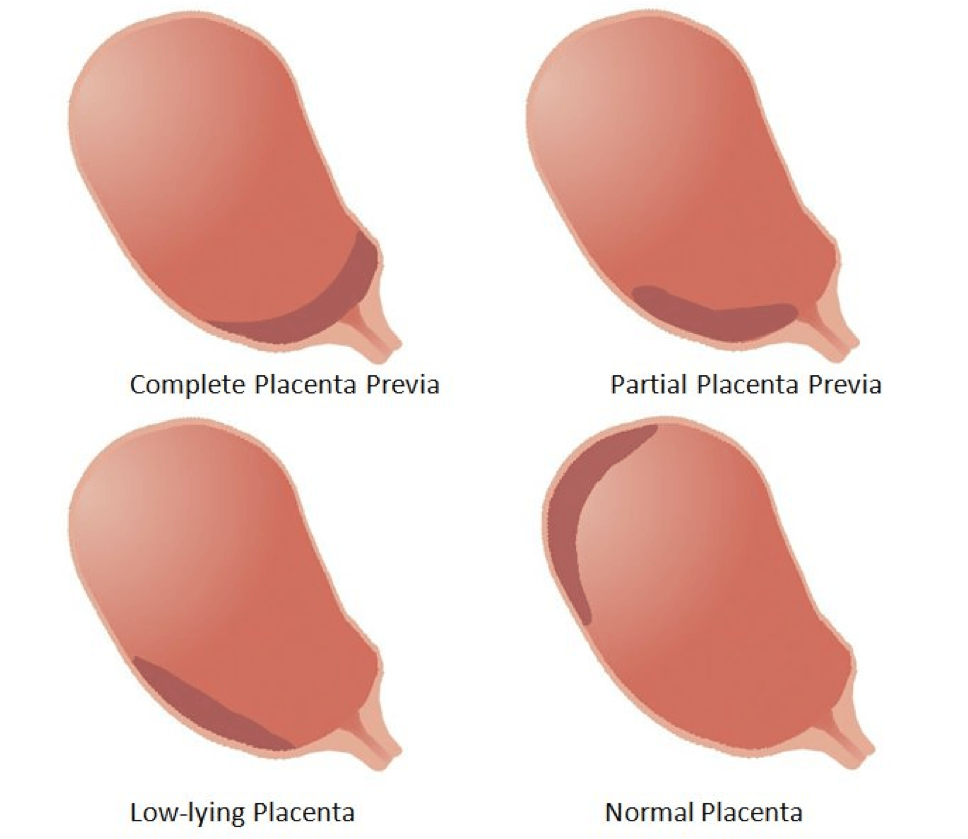
- Low-lying placenta: the lower edge of the placenta extends into the lower uterine segment;
- Partial or marginal placenta praevia: the lower edge of the placenta reaches to within 2 cm of the internal os (internal cervical opening that allows passage of the fetus);
- Major or complete placenta praevia: the placenta has a central location within the lower segment and completely covers the cervix.
Potential complications arising from placenta praevia include vaginal bleeding, preterm birth, and birth by Caesarean section.
Most episodes of vaginal bleeding are mild and stop by themselves. Bleeding should be assessed in hospital and may prompt admission until it has ceased. Occasionally, vaginal bleeding may be very heavy, occasionally requiring a blood transfusion. If bleeding is recurrent or does not settle, birth by Caesarean section is required, which necessitate a preterm birth. In a stable complete placenta praevia, Caesarean section will usually be performed at approximately 38 weeks.
Risk Factors
There is no single cause of placenta praevia. The following factors can increase a woman’s risk of developing the condition:
- Previous Caesarean section
- Advanced maternal age
- Multiparity (more than one previous pregnancy)
- Multi-fetal pregnancy (more than one fetus in the current pregnancy)
- Smoking
- In-vitro fertilization (IVF)
- Previous uterine surgery such as myomectomy, septoplasty, multiple D&Cs, lysis of adhesions for Asherman’s syndrome
Treatment
The first step is to do an ultrasound to define the type of placenta praevia. If placenta praevia has occurred in the context of previous uterine surgery, especially with multiple Caesarean sections, special consideration needs to be given to the possibility of an invasive placenta.
Uncomplicated placenta praevia crossing the internal os (internal cervical opening), but not causing any bleeding, does not require admission to hospital.
Many instances of minor placenta praevia can resolve during the third trimester. If the lower edge of the placenta is found to be at least 2 centimeters away from the internal os, then attempting vaginal birth is safe.
Women at home with major placenta praevia are advised to:
- Take a daily iron supplement to maintain their haemoglobin levels
- Avoid constipation (straining)
- Avoid intercourse
- Avoid highway driving (in case sudden bleeding were to occur)
- Remain within accessible driving distance or ambulance access to a major hospital
- Avoid travel to remote areas, or air/boat travel
Up to 50% of women with major placenta praevia will require admission to hospital due to bleeding before a planned birth date by Caesarean section. The additional precautions for major placenta praevia will include some or all of the following steps during their Caesarean section:
- Blood cross matched for transfusion
- Caesarean section will be performed 1-2 weeks earlier than normal
- A midline skin incision below the umbilicus (belly button)
- Midline (or classical) Caesarean section
- Additional skilled staff to assist
Maternal complications for a Caesarean section for major placenta praevia include the following:
- Need for general anaesthetic for the surgery
- Risk of requiring interventional radiology techniques to arrest excessive bleeding during the operating room after the Caesarean section
- Bladder injury at Caesarean section
- Caesarean hysterectomy (rarely needed to stop internal bleeding)
- Blood transfusion
- Need for post-operative admission to the intensive care unit
Health after placenta praevia
Mother’s health
Women who have an uncomplicated Caesarean section for placenta praevia should discuss their risk factors for recurrence at their 6-week post-partum visit.
Baby’s health
The main threat to the developing fetus is the need for early birth by Caesarean if vaginal bleeding is very heavy.
Future pregnancies
Women who have experienced placenta praevia are advised to defer pregnancy for more than 1 year to minimize future risks. They should have an early ultrasound at 12-14 weeks in future pregnancies.
